What is cirrhosis of the liver?
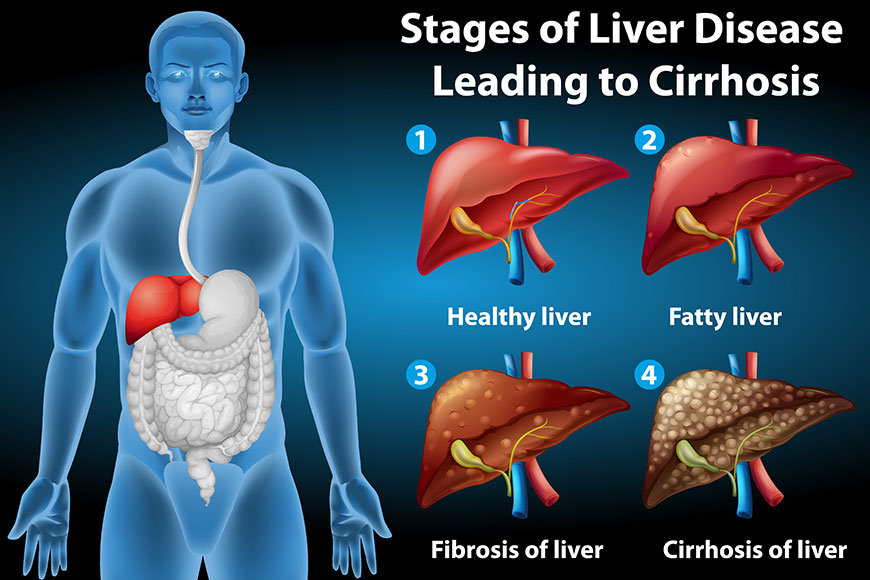
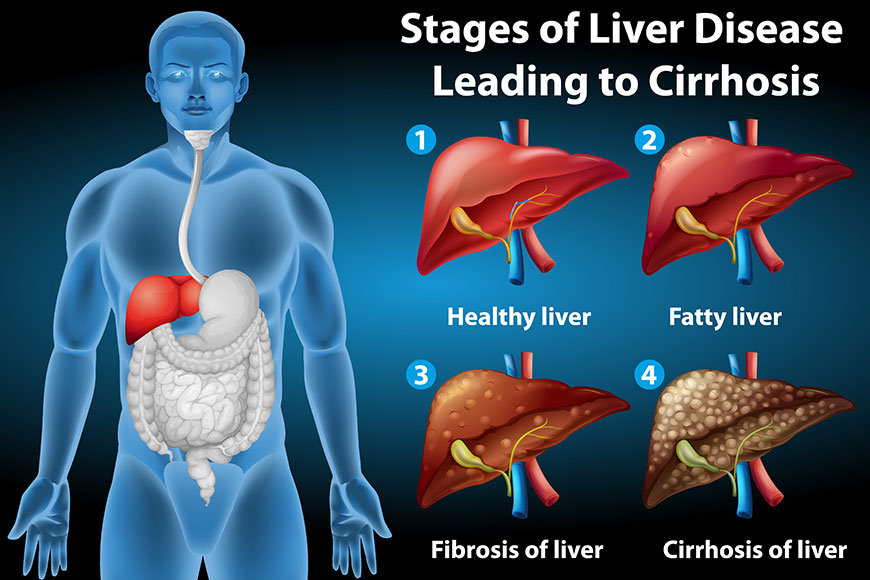
Cirrhosis is a late-stage liver disease in which healthy liver tissue is replaced with scar tissue and the liver is permanently damaged. Scar tissue keeps your liver away from working properly.
Who gets cirrhosis, who is most at risk?
You are more likely to get cirrhosis of the liver if you:
- Abuse alcoholfor many years.
- Have viral hepatitis/autoimmune hepatitis.
- Have diabetes.
- Are obese.
- Inject drugs using shared needles.
- Have a history of liver disease.
- Have unprotected sex.
- Have liver toxic drugs.
What are the symptoms of cirrhosis?
The symptoms of cirrhosis depend on the stage of your disease. In the beginning stages, you may not have any symptoms. If you do have symptoms, some are general and could easily be mistaken for symptoms of many other diseases and illnesses.
Early symptoms and signs of cirrhosis include:
- Loss of appetite.
- Feeling weak or tired.
- Fever
- Unexpected weight loss.
As liver function gets worse, other more commonly recognized symptoms of cirrhosis appear including:
- Easy bruising and bleeding.
- Yellow tint to your skin or the whites of your eyes (jaundice).
- Itchy skin.
- Swelling (edema) in your legs, feet and ankles.
- Fluid buildup in your belly/abdomen (ascites).
- Brownish or orange color to your urine.
- Light-colored stools.
- Confusion, difficulty thinking, memory loss, personality changes.
- Blood in your stool.
- Redness in the palms of your hands.
- Spider-like blood vessels that surround small, red spots on your skin (telangiectasias).
- In men: loss of sex drive, enlarged breasts (gynecomastia), shrunken testicles.
- In women: premature menopause (no longer having your menstrual period).
What causes cirrhosis?
The most common causes of cirrhosis of the liver are:
- Alcohol abuse (alcohol-related liver disease caused by long-term [chronic] use of alcohol).
- Chronic viral infections of the liver (hepatitis B and hepatitis C).
- Fatty liver associated with obesity and diabetes and not alcohol. This condition is called non-alcoholic steatohepatitis.
Other causes include Auto-immune Diseases, inherited disorders and some metabolic disorders.
What are the complications of cirrhosis?
There are many complications of cirrhosis of the liver. Because cirrhosis develops over many years, some of these complications may be your first noticeable signs and symptoms of the disease.
Portal hypertension: This is the most common serious complication. Portal hypertension is an increase in the pressure in your portal vein (the large blood vessel that carries blood from the digestive organs to the liver). This increase in pressure is caused by a blockage of blood flow through your liver as a result of cirrhosis. When blood flow through veins is partially blocked, veins in your esophagus, stomach or intestines can become enlarged (a condition called varices). As the pressure in these veins builds, the veins can bleed or even burst, causing severe internal bleeding.
Additional complications of portal hypertension include:
- Swelling (edema) in your legs, ankles or feet.
- Buildup of fluids in your abdomen (called ascites).
- Swelling/enlargement of your spleen (splenomegaly).
- Formation and dilation (expansion) of blood vessels in the lungs (hepatopulmonary syndrome), leading to low levels of oxygen in the blood and body and shortness of breath.
- Failure of kidney function as a result of having portal hypertension as a complication of cirrhosis (hepatorenal syndrome). This is a type of kidney failure.
- Confusion, difficulty thinking, changes in your behavior, even coma. This occur when toxins from your intestines aren’t removed by your damaged liver and circulate in the bloodstream and buildup in your brain (a condition called hepatic encephalopathy).
Hypersplenism: Hypersplenism is an overactive spleen. This condition causes quick and premature destruction of blood cells.
Infections: Cirrhosis increases your risk of getting and fighting serious infections, such as Spontaneous bacterial peritonitis (infection of the tissue that lines the inner wall of your abdomen).
Malnutrition: Your liver processes nutrients. A damaged liver makes this more difficult and leads to weight loss and general weakness.
Liver cancer: Most people who develop liver cancer have cirrhosis of the liver.
Liver failure: Many diseases and conditions cause liver failure including cirrhosis of the liver. As its name implies, liver failure occurs when your liver isn’t working well enough to perform its many functions.
How is cirrhosis of the liver diagnosed?
- Physical exam: Your doctor will examine you, looking for the signs and symptoms of cirrhosis including: the red, spider-like blood vessels on your skin; yellowing of your skin or whites of your eyes; bruises on your skin; redness on your palms; swelling, tenderness or pain in your abdomen; enlarged firmer-feeling, bumpy texture to the lower edge of your liver (the part of your liver below the rib cage that can be felt): enlarged spleen
- Blood tests: If your doctor suspects cirrhosis, your blood will be checked for signs of liver disease. Signs of liver damage include:
- Lower than normal levels of albumin and blood clotting factors (lower levels means your liver has lost its ability to make these proteins).
- Raised levels of liver enzymes (suggests inflammation).
- Higher level of iron (may indicate hemochromatosis).
- Presence of autoantibodies (may indicate autoimmune hepatitis or primary biliary cirrhosis).
- Raised bilirubin level (suggests liver isn’t working properly to remove bilirubin from the blood).
- High white blood cell count (indicates an infection).
- High creatinine level (a sign of kidney disease that suggests late-stage cirrhosis).
- Lower levels of sodium (is an indicator of cirrhosis).
- Raised level of alpha-fetoprotein (indicates presence of liver cancer).
In addition, other blood work will include a complete blood count to look for signs of infection and anemia caused by internal bleeding and a viral hepatitis test to check for hepatitis B or C.
- Imaging tests: Imaging test show the size, shape and texture of the liver. These tests can also determine the amount of scarring, the amount of fat you have in your liver and fluid in your abdomen. Imaging tests of your liver that could be ordered include computerized tomography (CT) scan, abdominal ultrasound and magnetic resonance imaging (MRI). A special ultrasound, called a transient elastography, measures the fat content and amount of stiffness in your liver.
- Fibroscan is alternative to liver biopsy
- Upper endoscopy to detect enlarged veins (varices) or bleeding in your esophagus, stomach or intestines.
Cure for cirrhosis of the liver?
No, there is no cure for cirrhosis. The damage already done to your liver is permanent. However, depending on the underlying cause of your cirrhosis, there may be actions you can take to keep your cirrhosis from getting worse. These actions include:
- Stop drinking alcohol.
- Treat chronic hepatitis (if you have it).
- Avoid medications that stress the liver.
- Eat a healthy, well-balanced, low-fat diet, such as the Mediterranean diet.
Follow other tips listed under the Prevention section in this article.
What are the goals of cirrhosis treatment?
The goals of treatment for cirrhosis of the liver are to:
- Slow further damage to your liver.
- Prevent and treat symptoms.
- Prevent and treat complications.
How is cirrhosis of the liver treated?
Treatment depends on what’s causing your cirrhosis and how much damage exists.
Although there is no cure for cirrhosis, treatments can delay or stop its progress and reduce complications.
Treatments for the causes of cirrhosis are as follows:
- Alcohol-related liver disease: If you’ve developed cirrhosis from alcohol abuse, stop drinking alcohol. If you need help, ask your healthcare provider for recommendations for alcohol addiction treatment programs.
- Hepatitis B or C: Several approved antiviral medications are available to treat hepatitis types B and C.
- Nonalcoholic fatty liver disease: Management of nonalcoholic fatty liver disease includes losing weight, following a healthy diet, getting physical exercise and following your provider’s instructions for managing your diabetes.
- Treatment of complications like UGI Bleed, Hepatic Encephalopathy, Ascites & Liver Tumors.
The Only treatment for end stage liver disease is liver transplantation.


